The universal tendency of age to be involved in the severity of the new coronavirus (COVID-19) and its reasons
The fact that the new coronavirus (COVID-19) is more likely to develop severe respiratory illness with the age is well known. This behavior is not specific to COVID-19 and shows a similar trend also in SARS and MARS that have occurred in the past.
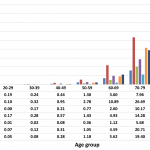
Below is the result of the latest COVID-19 fatality rates by ten-year age-groups in seven countries.
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0241031
The figure above proves splendidly that the elderly persons are really dangerous. But why does the fatality rate increase as the age increases? Unfortunately, we still don’t know exactly what the mechanism is for this.
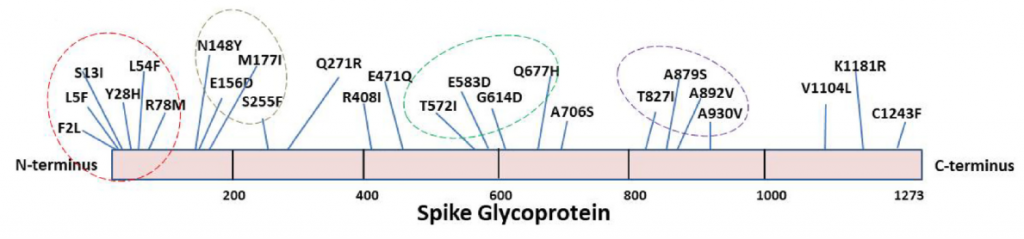
However, generally speaking, when the age increases, (1) dendritic cells and alveolar macrophages decrease, (2) the expression level of TLR7 and MDA5 is reduced, which are virus RNA receptors to activate innate immunity, and (3) although neutrophils and alveolar macrophages are on the increase, it can be said that the immune function of these cells such as phagocytosis etc. tends to decrease with the age. In other words, it seems to be a rough picture that the impaired innate and adaptive immune responses develops severe disease.
https://www.jci.org/articles/view/144115