The severity of influenza correlates with Host Cell’s high Mannose modification
For influenza viruses, it is well known that the binding of α2-6Sia in human respiratory tract cells and HA (hemaggulutinin) with influenza virus causes infection. However, the relationship between the severity of influenza and the glycosylation is not well known.
The following groups use lectin microarrays to study the severity of influenza and the glycosylation of Host Cells using ferret model.
https://www.pnas.org/content/117/43/26926.long
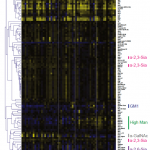
The result is that the glycosylation of Host cells changes when infected with the influenza virus, and the increase in the high mannose structure is correlated with the severity of the disease.
This is an interesting phenomenon. The high Mannose-binding C-type lectin is expressed on immune cells, so its association resulting in self-tissue damages might be suspected.