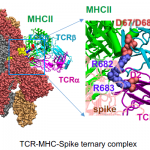
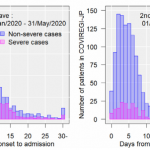
I also participate in a project targeting elucidation of the mechanism of the sever disease of new coronavirus (COVID-19) and the development of therapeutic drugs.
We promote development of this project by making full use of our experience and wisdom in glycans and lectins.
Thank you for your continuous support on our activities.
https://readyfor.jp/projects/glycotechnica_covid19research/announcements/150515