Identification of immune-related biomarkers associated with novel coronavirus (COVID-19) mortality
It has been established that cytokine storms are occurring in the severe case of covid-19, and there are many research studies about such changes in blood cytokine concentrations.
Some of the most noteworthy studies have already been introduced in this blog site.
- Report α cooperative effects of TNF-α and IFN-γ are causing severe diseases
- IL-10 is considered an anti-inflammatory cytokine, but may function as an inflammatory cytokine when it becomes more severe
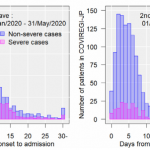
This article introduces the results obtained from covid-19 patients in Italy.
https://insight.jci.org/articles/view/144455
Clinical parameters indicate that the increase of the neutrophil/lymphocyte ratio, LDH, CRP, and D-dimer correlates with mortality.
In this study, 66 types of cytokines in the blood were evaluated, suggesting that MCP-1/CCL2, sTNFRSF1A, MMP-9, NGAL, S100A9, sST2, IL-10, and IL-15 were deeply related to the serious disease of COVID-19.
As a site note,
MCP-1/CCP, sTNFRSF1A are NK-kB-dependent markers,
MMP-9, NGAL, S100A9 are derived from neutrophils,
sST2 is a septic marker,
IL-15 is associated with NK-cell activation and function,
IL-10 is a counteraction of severe pneumonia,
has been discussed as such.
As the mechanism of serious disease becomes more concrete, effective therapeutic drugs will be narrowed down.